Episode 4 of the Underbelli: Beyond Psychiatry and Self-Care – Approaching New Pathways in Mental Health
This episode is comprised of a reading Sasha Durakov did first in Minneapolis in July and then in Chicago in August, with some minor changes to account for the switch to an audio format. The description read:
‘Many of us are familiar with some ideas, images, or theories of madness, “mental illness”, and perhaps also psychiatry, but feel a lingering skepticism and doubt about what they mean. In this episode, we will attempt to challenge common beliefs about mental health; present the problem of madness in an open, nuanced way informed by the voices and stories of people with lived experience; and to introduce the audience to alternative ways of responding to and approaching madness and to provide the materials and direction to help foster new discussions and practices in mental health (and hopefully some reading groups!).
Go here for the free study guide.’
What follows is a transcript of the episode, with some minor changes made during the editing process. Check the study guide for the sources used for the creation of this reading. Also included are some images I used during the events. Listen to the episode wherever you get your podcasts, or go to this link:
Transcript of the episode
Welcome to the Underbelli. My name is Sasha Durakov. What follows is reading from a text I wrote for and read at an event in Minneapolis in July, and Chicago in August called “Beyond Psychiatry and Self-Care: Approaching New Pathways in Mental Health”. The text is partly a culmination and summary of my last few years of research and reading, but more so a reckoning with events and understandings of the past and present. I also presented an annotated bibliography, which I’ll properly introduce you to at the end, so stick around. This reading is in three parts. Each of the readers for this episode has had experience in the psychiatric system, two as patients, one as a service provider.
I. Approaching Madness
In which I’ll argue that the way we approach mental illness is dominated by a number of cultural and scientific presuppositions, which need to be challenged before we can even begin to talk of “alternatives”.
Have you ever asked yourself how many angels can dance on the head of a pin? While it’s debatable that any of the theologians of the Middle Ages ever actually asked this question, it’s become a sarcastic allusion to the reality that the learned doctors and men of science in Europe asked many such questions for hundreds of years, filled books with them, and became the most respected scholars for generations.
More recently, just 150 years ago, the Hygienists reigned supreme in Europe and were considered the most trusted and necessary of health professionals. These Hygienists made it their mission to bravely venture out into the decrepit hovels of the ragpickers and the infested brothels of sex workers to find out why tuberculosis, venereal disease, and leprosy made its eternal home with the poor, as if the shadow of the working classes formed the gaseous outline of the four horsemen of the apocalypse on the horizon.

These men of science made two empirical observations: one, that lepers, poor people, and sex workers smell rotten; and two, that those who stink are carrying a disease. This observation turned into science when they discovered that they could classify such smells into a detailed diagnostic system: if you smelled like semen and musk, you are a homosexual and carrier of venereal disease; if you smell rotten, you are a ragpicker and likely a victim of tuberculosis. The smell was not an effect of the disease, but its cause.
That we now laugh at these geniuses of the past and consider their practical conclusions absurd is irrelevant. What is revealed by these two examples is that neither the accumulation of detail and fact, nor the trust we place in experts, nor empirical correlation are the foundation of certain truth. Science at all times claims to be a steady island at the center of a tempestuous ocean; a valueless place of pure, positive discovery and neutrality. In this image, scientists spend their days peering behind bushes in an empty field called knowledge, discovering to everyone’s benefit that a disease lives there for anyone to see.
Keep that in mind as we consider a number of facts about mental health. The number of people who are diagnosed with a mental disorder is steadily growing every year, especially when looked at globally. According to the World Health Organization (WHO), over 450 million adults have a diagnosable mental disorder worldwide. They also report that the number of suicides increased by 60% over the last 45 years. So, what are the possible conclusions from this? Something must be done, right? We need “more mental health services”, as many activists and others are apt to say. But what does that actually entail? Access to medication? Yoga classes? More hospital beds? Free or affordable therapy? Special psychiatric security officials? The return of the asylum?
Calling for “more mental health services” starts to look somewhat questionable when one looks at a number of other facts. In the 1970s, WHO conducted a global five-year study in which they found that those diagnosed with schizophrenia —usually considered the most debilitating of all mental disorders— fared better in developing countries than in the U.S. In three of the developing countries in the study —India, Colombia, and Nigeria— only 16% were on antipsychotics, the first line of treatment for schizophrenia cases in the US and Europe. In a repeat of this study, they found the same results, and concluded that living in a developed country was a “strong predictor” that a person would never fully recover. A number of follow-up studies found that patients who had weaned themselves off the antipsychotics, which were said to “fix their brains by correcting an imbalance” had actually fared better than those who continued to take them. When faced with this second set of facts, the idea of mental health treatments being a human rights issue starts to break down.
How do we examine or compare such facts? Do we examine them in relation to all the studies that have been done on psychotropic medication, on hospitalization, and on therapy and simply choose to fund the means with the highest number of “recovered patients” at the end? A number of questions get lost in such an analysis, questions beyond the scope of these studies, questions which perhaps trouble the foundation and presuppositions of the studies themselves. For example: how does one get diagnosed as schizophrenic or bipolar? This isn’t a question about symptoms, but about power. Who does the diagnosing? With what tools? How are these tools legitimated? Against what standard is mental or emotional pathology measured? How did the person getting diagnosed end up in their position? What does it mean to recover from such conditions? And, most importantly in my eyes, what is the concrete experience of the mad person in these relationships?

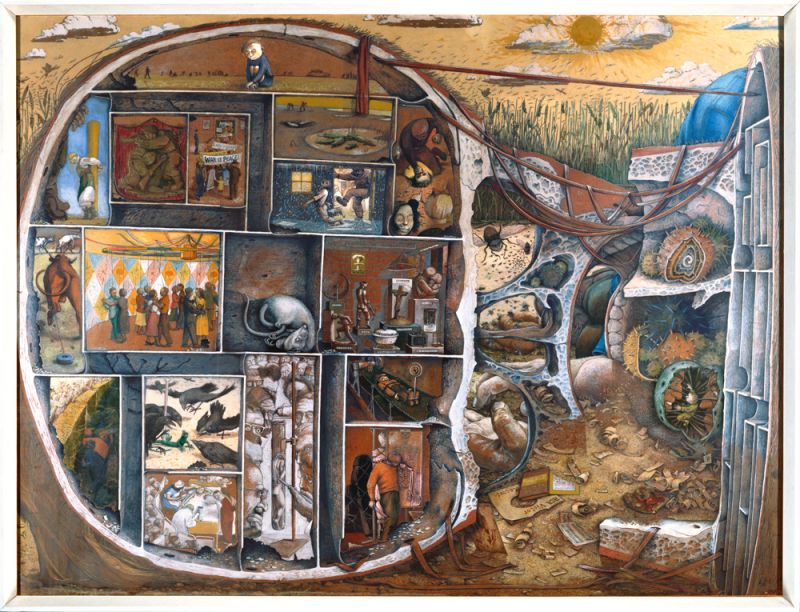
I Spit on Life by William Kurelek
In Sylvia Plath’s book “The Bell Jar”, the narrator, Esther —a stand-in for Plath— often considers suicide when she is forced to move back and live with her mother again. She tries hanging, drowning, pills, but nothing seems to work. At the peak of her desperation, she finds herself socially coerced into spending time with peers who have no idea what she’s experiencing. One of these peers talks incessantly about a play. Plath writes
The only reason I remembered this play was because it had a mad person in it, and everything I had ever read about mad people stuck in my mind, while everything else flew out…
Plath or Esther wants merely to reflect on her madness, on her morbidity and longing for death. She wants to know others who have experienced such states of mind and find out what happened to them. It’s one small glimmer of the fire for living otherwise extinguished at this point in her life. She doesn’t find such people, and she can find no such stories. What she does find is a textbook on abnormal psychology, and at her absolute lowest point, she explains her desperation in the following way
my case was incurable. I had bought a few paperbacks on abnormal psychology at the drugstore and compared my symptoms with the symptoms in the books, and sure enough, my symptoms tallied with the most hopeless cases.
If Plath had been alive today, she may have found one of many patient-centered groups, and groups of those who identify with unusual experiences typically seen as “crazy” (hearing voices, extreme mood shifts and expressions, seeing things, having “strange beliefs”) who are organizing themselves in social groups, study groups, support networks, and activist groups. The mere existence of such groups already wears upon the more extreme claims made by psychiatry that, for instance, unmedicated “psychotic” patients will flounder in their undertakings and live solitary lives trapped in a world of fantasy. If such people were able to form international social, support, activist and political groups, something is amiss about those claims.
But before we get to stories and theories of madness, of psychiatry, or of “mental illness”, we have to address something more fundamental: people feel very strongly about “mental health”, even (or maybe especially) when they do not have a definition for it. Worse still is that the noble language of “abolishing stigma” has by and large been appropriated by the proponents of the medical model, creating a situation in which all mental health activism is assumed to be part of a movement to make psychiatric diagnoses and treatments more acceptable, which is patently not the case. The opposite of stigma is not the act of admitting to illness.
The confusion around mental health revolves around the fact that, despite what nearly everyone is saying, the problem is not that people don’t know enough or don’t have enough information or awareness about it. The world feels over-saturated with ideas, facts, and awareness weeks about mental health. This “ever more facts” model serves above all to bury the essential problems related to madness under a mountain of details. The problem then is that people feel like they know enough to make definite claims or actions about mental health. That confidence in the ability to identify mental illness, and use words like “depressed,” “psychotic,” or “anxious” to describe others or ourselves; the self-deputization to diagnose friends, family, or someone on the street; the comfort with calling the police or a psychiatric crisis team when faced with something unexpected or extreme are indications that we actually have profound confidence in one particular understanding of what “mental illness” and “madness” can be. When the public space for dialogue is so crowded with contradictory scientific theories, with rhetoric of terror around violence and mental illness, and with pharmaceutical solutions, it leaves no space for new approaches, let alone the space for the mad to tell their own stories in the depth and complexity they require. When someone becomes so certain that they know enough about mental health, when they’ve reduced the range of possible experiences of madness to a set of diagnoses in a book, they cease to be receptive to different ways of experiencing and organizing the reality around them. If you are so invested in researching whether or not the angels dancing on the tip of a needle must wear shoes, or classifying which mental disorders your favorite cartoon characters likely have, you are surely missing the important questions like “is this actually important or helpful?” and “do I even believe in the angels or the diagnoses at all?” We need concepts that help us cut through the fog as a lighthouse does over the shore, so that we may find our way in this infinite sea, at least at moments.

The Death of Pentheus, red figure kylix from Athens, c. 480 BCE; terracotta; painting attributed to Douris
So let us discuss madness. Experiences, ideas and concepts of madness predate psychiatry by hundreds, if not thousands, of years. People throughout history have talked about, theorized about, respected, feared, and treated madness. The history of madness up to the birth of psychiatry is truly an impossible history, for there is no consistent subject nor object to trace. It is not a linear history beginning from some primitive understanding of madness, slowly evolving into modern day psychiatry. Without retroactively applying contemporary psychiatric diagnoses, like depression or schizophrenia, on people in the past, all we have available to us is who was called mad, by whom, and why. Madness, if we want to talk about it as something that extends centuries, cannot be represented by a class of people, nor by sets of symptoms, since these have shifted so often and so dramatically. Instead, looked at historically, madness has represented at almost all times both a relationship of power and a possibility of experience. Historically speaking, madness exists between people, not within them. This complex interplay between the experimental forms of communication and thought called madness on the one hand, and the acts of authority and diagnosis implicated in seeing the Other as mad are what make madness impossible to pin down definitively.
In Ancient Greece, the prophets who convulsed and told of wars and famines to come were called mad, as were the artists and philosophers who envisioned new ways of thinking about or representing the world. Socrates called madness the greatest gift. This is madness as the possibility of having novel experiences closed off to reason and normality. Now consider a play like “The Bacchae” by Euripides, also from this era. The Bacchae were the female followers of the god Dionysus, the god of wine, theater, illusion, and madness. The play features a male character named Pentheus who refuses to honor Dionysus, believing solely in the power of reason, who is punished by being torn to shreds by the bare hands of the Bacchae. This play would have been a scandal at that time, as the men thought of themselves as the only ones untainted by irrationality, and thus the only ones reasonable enough to govern. According to them, women, slaves, and foreigners operated more so on base instinct, emotion, and impulse. The men, as they have at nearly all times, defined themselves by their ability to reason in distinction to the mad, irrational subjects. Thus, this play marks one of the first cultural documents in the West to make the connection between the mad, and everyone else excluded from patriarchal civilization. Women and slaves were akin to mad people in that all of them were considered to be incapable of correctly reasoning as the “civilized” do. For any civilization whose members define themselves by their ability to use reason, madness becomes a symbol of exclusion. The mad are those who cannot reason, and only the reasonable can be included.
These two trends evolved and branched out over the years. Sometimes, they coalesce into a single, dramatic event as when the English poet Nathanial Lee began to write increasingly extravagant plays critical of the king until they eventually sent the authorities to have him dragged off to infamous Bedlam Asylum in 1684. He is quoted as having said “they called me mad, I called them mad, and damn them, they outvoted me.” In the Middle Ages, there was a profound ambiguity between who was “mad” and who was a divine prophet. Further, many Christians considered the ravings and frenetic behavior of vagabonds and the insane as a religious trial, who were thus respected for being in the middle of a spiritual journey. Somewhere around the 16th century, a new police force arose which was allowed to arrest without distinction the mad, the poor, the decrepit, the unknown, and the unwanted and put them to work in poorhouses, or place them in hospitals, which gradually morphed and reformed into the asylums of the 20th century. Many of the classic images of the mad come from the early period of incarceration when lunatics were put on display like circus animals in Germany, England, and later in the US for people to gawk and throw stones at. At the dawn of the modern era, in the 17th century, when melancholy was fashionable among the literary class in Europe who believed it gave them access to special insights, the French doctor De Laurens, and the English doctors Thomas Willis and Richard Mead made concrete the connection between colonized and foreign subjects with the mad when they theorized that both share a mental constitution more so resembling an animals than a humans. Willis wrote this about melancholy for instance in “Two Discourses concerning the Soul of Brutes”
as Melancholick people talk idly, it proceeds from the vice or fault of the Brain, and the inordination of the Animal Spirits dwelling in it.
Madness is best described historically as a term of relation that can describe either novel, unusual or extreme experiences of those who are called or call themselves mad or within the operations of a class with power who names another class delusional and mad. It hasn’t so much evolved as broken apart and leapt around. What is special about that last quote, and what makes it a text of proto-psychiatry, is that it collapses all the different former possibilities of madness and crystallizes them into a single biological, and invisible process in the individual. With this new language, it claims to explain every former instance of madness in a dramatic bid to, in effect, erase the history of madness, so as to inaugurate the history of mental illness.
II. The Psychiatric Era
In which I will question the psychiatric hegemony over the idea of madness, and the way it has reduced its possibilities to mean only mental illness.
Sometime after the French Revolution, around 200 years ago, there came into being a group of doctors (iatros) who began to exclusively study and treat the mind (psyche). Psyche-iatros, psychiatry. We can conclude from our brief historical survey that madness and psychiatry as we know it are not essentially related to one another; the latter represents one possible response to what is called “madness,” yet one that is becoming globally dominant as a language of explanation and as the first line of treatment as it continues to export its diagnostic labels and psychotropic medication into the global south. One of the central powers of psychiatry, and the activity that separates it from previous explanatory regimes, is the ability to define what madness is, concretely and physically, or, in contemporary language, what a “mental illness” is, and also to classify —and thus simplify— their manifestations into a classificatory system (a “nosology”). Psychiatry, then, reduces the possibilities of madness to just one: mental illness.
Psychiatry claims, like any branch of medicine, to have discovered positive and real diseases, which it purports to treat. But psychiatry is not like other branches of medicine for a number of simple reasons: First, its categories are based on notions of normality, and thus are contingent culturally and historically, which we’ve briefly touched on. We’ll come back to this. Second, it now claims to study “brain diseases”. This can’t be said to be literally true. When neurologists discover the biological roots of a disease in the brain, it largely ceases to be considered a psychiatric disorder and becomes a neurological problem. This has happened with epilepsy, the various forms of dementia, Down’s Syndrome (which used to be called feeble-mindedness) and is now happening with autism spectrum (Here, I am not implying that autism nor Down’s Syndrome are “disorders” but merely remarking on where they land in scientific literature). Far from bolstering or combining with psychiatric knowledge, as many hoped, the growth of neurology has pushed psychiatry into the defensive. Third, and connected with the second point, psychiatry is the only medical branch I can think of that has its fundamental concepts and diagnoses consistently put into question, and not just by its detractors, but by its proponents as well. I can’t think of any respected doctor alive today who would deny the very existence of cancer, or diabetes, yet there are respected psychiatrists working within the hospital system like Jim van Os who publicly deny the existence of schizophrenia, bipolar, and others. Nor can I think of any anti-cardiologist or anti-rheumatologist activist groups, and yet we have a global and historical anti-psychiatry movement. Why?
The clearest way to approach this problem is through the tool psychiatrists and some clinical psychologists use to make a diagnosis. Diagnosis is arguably the most contentious power in the toolbox of psychiatry, and also its source of authority. If the physician could not make authoritative claims as to who is mentally ill or not, then they would have no power to treat. In America, this tool is called the DSM, or the diagnostic and statistical manual, now in its fifth edition. The DSM is an extremely important document, which has changed millions of peoples lives. It’s important for legal reasons, as many may not receive any services unless they meet the criteria for a diagnosis, and because it can affect your status in a trial; it’s important for insurance and billing purposes, as many mental health professionals need to dole out a diagnosis if they want to be legitimate in the eyes of the state; it’s also important for subjective purposes, as many in a state of crisis or confusion seek out authoritative explanations that help them make sense of their lives.
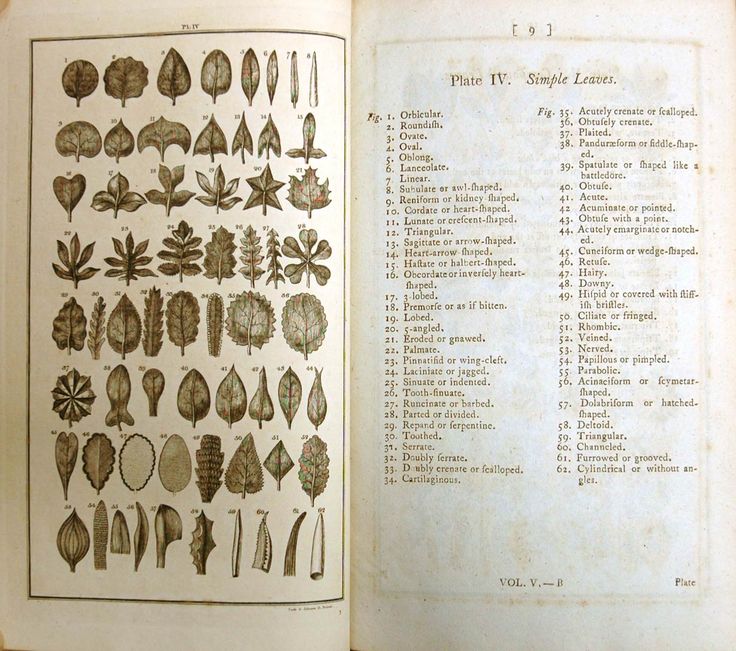
A page from Linneas’ Classes Plantarum and Bibliotheca Botanica
It is based off of the German psychiatrist Emil Kraepelin’s 1883 textbook “Compendium of Psychiatry: For the Use of Students and Physicians”. There, he treated the psychiatric understanding of mental illness as being like botany (and his brother Karl was a famous botanist): the goal was to classify all the different types into their correct generic orders and species. No psychiatrists before him attempted such a systematic approach. He established many trends in his book, which would come to dominate psychiatry up to today: the major distinction between affective and psychotic disorders comprising the major “types” of madness; the emphasis placed on psychosis as a measure for the severity of the illness; and the strange mixture of confidence that a biological explanation is soon to come coupled with the admission that they do not yet have one.
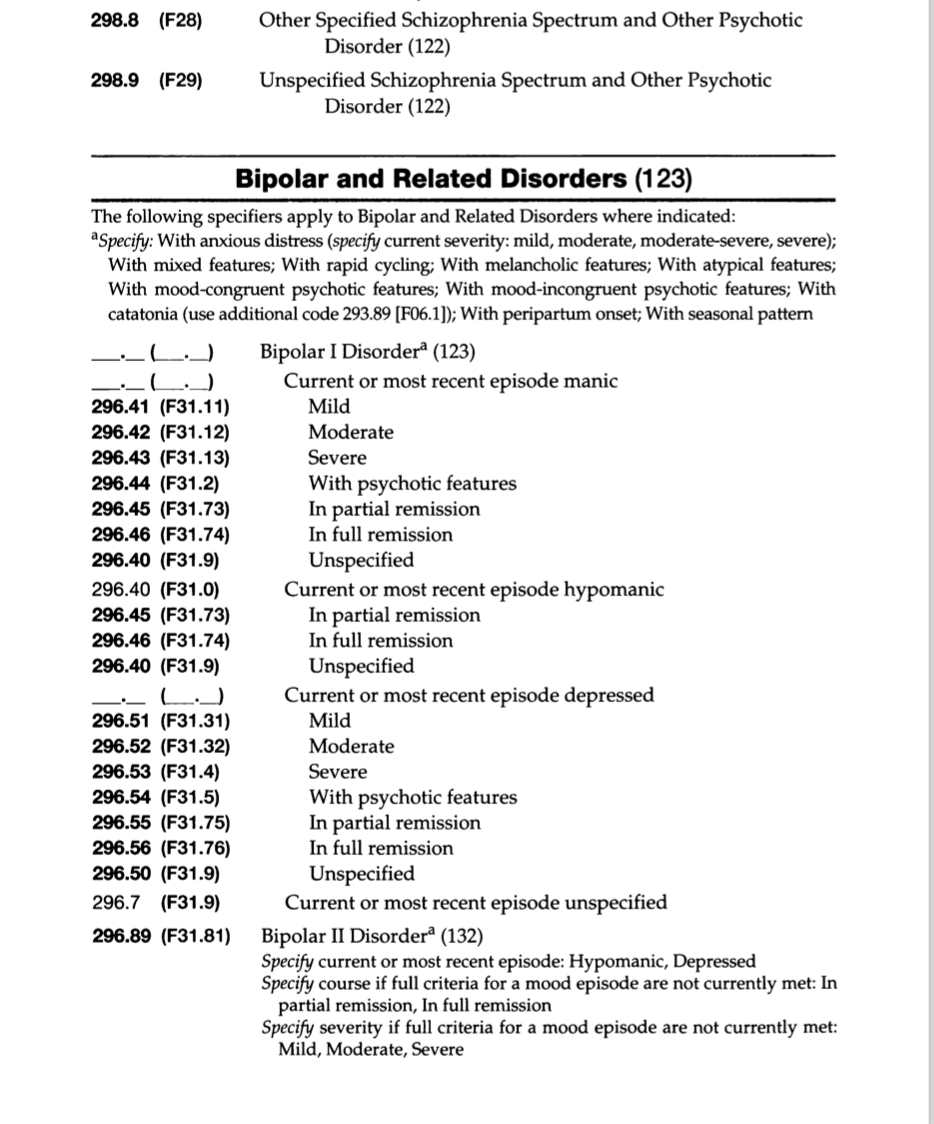
DSM-V page on Bipolar disorders
Ask yourself whether you think the following diagnoses have appeared in either an edition of the DSM or in another official clinical manual of psychiatry. We’ll start with the easy ones: Schizophrenia? Major Depression? Bipolar disorder? How about Inadequate Personality Disorder? Oppositional Defiant Disorder? Masturbatory Psychosis? Gender Identity Disorder? Caffeine Withdrawal? Old Maid’s Disease? Hysteria? Homosexuality? Perhaps you will find it surprising that all of these have appeared at one time or another. I would hope every person listening to this would derisively view Hysteria and Homosexuality as nothing more than medical codifications of the male doctors internalized homophobia and misogyny. But, according to psychiatric dogma, the diagnoses in their manuals are real diseases they have discovered. Does it not seem odd then that the American Psychiatric Association votes on which diagnoses to include in their new additions? This is ultimately how homosexuality was eventually ousted in the wake of a number of protests by gay rights activist groups. “Homosexuals gain instant cure!” read a a humorous headline in 1973. Do you imagine that the editors of medical textbooks on cancer voted as to whether to include ovarian cancer in their newest edition? The situation is made worse by the fact that the leaders of the last two task forces of the DSM, essentially the editors of the most authoritative diagnostic book in global psychiatry, Allen Frances and David Kupfer have made public statements declaring the continued lack of biological evidence for the diagnoses. Kupfer, the head of the task force for DSM-5 has said in a statement in 2013
The promise of the science of mental disorders is great. In the future, we hope to be able to identify disorders using biological and genetic markers that provide precise diagnoses that can be delivered with complete reliability and validity. Yet this promise, which we have anticipated since the 1970s, remains disappointingly distant. We’ve been telling patients for several decades that we are waiting for biomarkers. We’re still waiting.
One need not have professional knowledge to know that psychiatry is indeed like no other profession if Thomas Insel, the director of the National Institute of Mental Health, can announce, as he did in April, 2013 that he believes DSM categories lack any scientific validity or objective measure.
Many people likewise assume that psychiatry and psychology are basically on the same page, in the way that a cardiologist and a nutritionist might be in basic agreement about your state of health but merely offering to explain different aspects of it. This is quite far from true. This is clear from the petition leveled against the DSM 5 by the American Psychological Association and from the statement and table put out by the British Psychological Society, an organization of around 50,000 psychologists in the UK, following the publication of DSM-5 in which they wrote
The putative diagnoses presented in DSM-V are clearly based largely on social norms, with ‘symptoms’ that all rely on subjective judgements, with little confirmatory physical ‘signs’ or evidence of biological causation. The criteria are not value-free, but rather reflect current normative social expectations.
Diagnostic systems such as these therefore fall short of the criteria for legitimate medical diagnoses. They certainly identify troubling or troubled people, but do not meet the criteria for categorization demanded for a field of science or medicine.
The question we all must confront in ourselves at this point is: why do I feel so confident using psychiatric vocabulary and feel the need to do so when even professionals in psychiatry and psychology (not to mention the many others in sociology and anthropology) can’t seem to agree on what mental disorders are, or at least have expressed serious doubts as to their ability to identify them? What exactly does diagnosing allow you to do? Without referencing anyone in particular, I think it must be squarely faced that many average citizens feel a sense of relief in being able to say “there are just crazy people out there.” This imaginary citizen does not have to confront whether he has done something to frighten, traumatize, or provoke the mad person; he need not worry that he has not yet confronted the horrors of slavery and violence in his country’s history and the way they live on today; he need not concern himself with the idea that perhaps there are other ways of thinking about the world that do not align with his own. Calling someone on the street acting bizarre or the mass shooter in the news mad serves the function of easing the contemporary citizen’s anxiety about the uncertainty of the world. “There are just crazy people out there, it’s something in their brain” he repeats to himself like a mantra, and his world-view remains in this way untainted and unthreatened by anything outside of it. In order to even begin to have a conversation about madness or mental illness, we need to see that we feel that we know more than we actually can know about madness, confront why we desire to wield the coercive power of diagnosing, and begin from that careful skepticism and admission of impossibility.
The question of why mental health professionals use categories of mental illness so often put into question is much simpler to answer. The most obvious reason is that mental illness, as opposed to madness, is marketable. One can sell pills to manage the former, but there is nothing to sell someone suffering from the effects of capitalism. The second is that their categories are predicated on a conflation between normality, health, and morality. The poet and madman Antonin Artaud explained the underlying magnetic drive towards normality in psychiatry in his own furious and frenetic way, clearly influenced by the imprisonments and insulin shock treatments he had been forced to withstand. He said: “Medicine is born of evil, if it is not born of disease, and it has even, on the contrary, provoked sickness out of whole cloth in order to give itself a reason for being; but psychiatry is born of the vulgar soiled earth of people who have wished to maintain the evil at the source of illness.” Artaud is not implying that medicine and psychiatry are themselves evil, but that they come into existence when professionals feel they have discovered some evil which needs to be rectified.” In mental health, this becomes more complicated, since the “evil” in question is not the destruction of the body by a discrete disease or plague, but of behavior, emotional expression, and thinking. A cartoon drawn by Emil Kraepelin in the 1850s shows Kraepelin himself clad in the armor of an arch-angel, wings spread out behind him declaring “Psychiatrists of Europe! Defend your sacred diagnoses!”

Hiawatha Asylum for Insane Indians
Psychosis is defined by the presence of supposedly unreal phenomena like hearing voices, or seeing visions, and the belief in unreal truths. This definition ought to make anyone familiar with American history feel uneasy. Was not slavery considered completely normal in this country, along with the idea that black people and natives were closer to animals and only partly human? So too was expropriation, genocide, and cultural theft and destruction of the Native perfectly aligned with the program of a nation whose aim was to “kill the Indian” and “save the man”. In such a case, how, for instance, is a white psychiatrist supposed to diagnose a Native Dakota Indian without speaking her language, understanding his customs, ways of acting or speaking? How could a physician diagnose a mental illness when another people’s entire way of being in the world is a problem in their eyes? Pemina Yellow Bird writes in “Wild Indians: Native Perspectives on the Hiawatha Asylum for Insane Indians” that ‘Native peoples generally do not have a notion of “insane” or “mentally ill.” I have been unable to locate a Native Nation whose indigenous language has a word for that condition. The closest I can come is a word more closely aligned with “crazy,” which means someone is either very funny, or too angry to think straight.’ And yet they did, and do, at extraordinarily high rates beginning with the Hiawatha Asylum for Insane Indians in the late 19th century when hundreds of Native peoples were sent from hundreds of miles away, incarcerated and punished for practicing their religion, performing dances, or speaking their native languages and forced to speak English. Most patients, or prisoners, went undiagnosed, and were just called “insane” or “defective”, after which they were sterilized and kept until the end of their lives. Nine out of ten discharges were due to death. Today, American Indians have the highest rate of serious and minor mental illness besides multiracial individuals, according to the National Institute of Mental Health. In our second episode “The Madwives’ Blues”, we discussed the schizophrenic women of the 1950. At that time, schizophrenia, the disease most characterized by psychosis, was a disease mostly attached to the disorderly wives of white men who were then placed in asylums and given shock treatments. The schizophrenic woman was the wife or single woman whose delusions were were characterized by their doctors fantasies about sleeping with the neighbor, or running away from home. One advertisement for the antipsychotic Zyprexa portrays a woman with a puzzle piece shaped hole where her mouth should be. The text reads “You’re trying to piece her life together, but she won’t swallow it”. Similar stories can be told about homosexuality, the history of the treatment of transgender people, women through the diagnosis of hysteria and personality disorders, with the rebellion of children through oppositional defiant disorder and emotional behavioral disorder, and colonialism through psychotic disorders.
1967 ad for Thorazine
Psychiatry also provided, along with the burgeoning field of genetics, the intellectual and clinical backbone of the eugenics movement in the United States, and later in Nazi Germany. The father of psychiatry, Kraepelin himself, was a eugenicist who believed genetic cleansing would finally restore the great german people tarnished by the insane and disabled. Mothers with deficient heredity were sterilized well into the 20th century, people with disabilities and those acting mad were incarcerated, subjected to experimental treatments against their will, and, in the case of Germany, murdered en masse. Individuals labeled schizophrenic were the first to be gassed in Germany, having been deemed the most expendable and least likely to be missed in the gene pool. Eugenics is the logical and final outcome of the total overlap between medical science and the moral drive for normalization, and one which we are never entirely safe from. Much of the language we use to talk about our minds and emotions comes from this era. The term “mental health” itself arose from the American eugenics and mental hygiene movement.
What we must take away from these examples is not that past displays of rebellion and radicalism were being misunderstood or misconstrued as psychosis, but rather that they were indeed psychotic in the terms defined by psychiatry. A world unaffected by white supremacy, by patriarchal violence, by the legacy of colonialism or capitalism is unreal, and to imagine it is dangerous, aggressive, and delusional to those who decide what’s medically reasonable. Normality is whatever is made normal, through language and culture, yes, but also through political maneuvering, armies and economic structuring; psychiatry allows those who see themselves as normal to recast the abnormal as not just different, but “sick” and “delusional”, unworthy to even listen to. In fact, a symptom of many mental illnesses today is “anasognosia” or “lack of insight into condition”. If you visit an asylum’s graveyard in New York, California, Illinois, or any other state in this country, you will likely find gravestones marked with number, not a name, because those buried there were not considered individual human beings at all. This was the case in Minnesota as well until the disability group Advocating Change Together did the research in the 2010s to find 7,000 of the near 15,000 anonymous buried on Minnesota’s asylum properties.
This is why mental illness is not “like any other illness” or “breaking a leg.” If I break my leg, my words and actions, or even my human status will not be put into question, I will not be carried away by the police, drugged or held against my will, nor will I have to bear the stigma and erasure imposed by a psychiatric label. Anosognosia implies that those labelled as mad are the last people we ought to seek guidance from and that there is nothing to learn from the content of their speech. Truly listening to those called mad and those we think of as mad is thus from the outset a political stance, in that you are demonstrating by doing so that you hear in their language more than word salad and the expression of abnormal brain chemistry.
To close part two, I’d like to say that self-care strategies are necessity for mitigating the effects of our distress, and for staying healthy in this toxic world, but if your self-care paradigm is based off the idea that the problem with the medical model is that schizophrenics ought to be substituting Haldol for St. John’s Worth, then the broader paradigm of care remains unchallenged. I acknowledge also that some people have had good experiences with a medication or a psychiatric treatment. In my experience, many of those people sought out their diagnoses and treatments voluntarily. I would only say that this does not warrant making these individual experiences grounds for a social program, in the same way that someone meeting a nice police officer cannot serve as a counter-argument to critiques of policing or the police. This comparison is particularly useful since, in the absence of clear or consistent scientific legitimacy or validation, psychiatry appears historically to more closely resemble a police force than a medical science.
III. Listening to the voices
In which I will show that it is from the mad themselves where we could learn true mental health alternatives, if only we were able to hear them.
At long last, it’s time to celebrate the works of the mad, the lunatics, and the crazies. I will briefly and quickly show the various movements and trends in the mad movement around the world with the hope that you will follow up on whatever resonates with you.
But who are the mad we ought to listen to? Without implying that they are in any way separate from one another, the literary, social, and political expressions of the mad have generally followed the two pathways we indicated earlier: the work either appears as a novel form of expression outside of the norms of an era; or it situates itself as a response to the real repression of what is called madness through incarceration, forced diagnosis and medication, stigma, and mistreatment. Within these two possibilities, we’ve already seen even in my brief exposition myriad ways in which madness can appear: madness as deviance, madness as extreme suffering or elation, madness as scapegoat, as disease, as difference, as spiritual emergence and connectedness, and madness as inspiration or genius. These are nearly always implicated in one another, twisting and winding about in each others soil like so many ecstatic fungi.
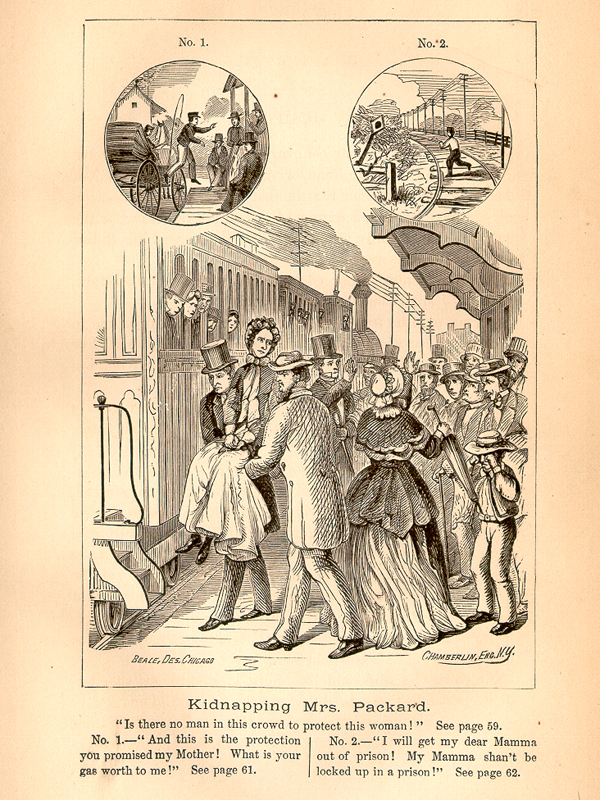
The mad people who have been locked up, medicated, or “treated” without their consent or under premises they later saw as false have created a global “psychiatric survivor” movement that spans over a hundred years. An early organization for psychiatric survivors came to be right here in the Midwest, when Elizabeth Packard was diagnosed as mad and put into the Illinois State Hospital for the Insane when she disagreed with her husband’s Calvinist religious doctrines. Some of the signs of her insanity included not wanting to shake his hand, and preferring Methodist Christianity. Once her son was able to get her out, she wrote multiple books on the incident and started one of the earliest psychiatric survivor groups: the “Anti Insane Asylum Society”. The 1970s saw a resurgence of patient-led groups undoubtedly inspired by the Black Power, feminist, queer liberation, and especially disability movements of the era. One of the major figures was Judi Chamberlin, who, following her involuntary hospitalization in 1966 for schizophrenia following a crisis after a miscarriage, helped form the Mental Patients Liberation Front. She wrote that “Only when a group begins to emerge from subjugation can it begin to reclaim its own history…The movement of people who call themselves variously, ex patients, psychiatric inmates, and psychiatric survivors is an attempt to give voice to individuals who have been assumed to be irrational – to be out of their minds.”
David Oaks, also a member, went on to form MindFreedom International, a large coalition against forced treatment with chapters in the UK, Africa, and elsewhere who focus on documenting psychiatric abuse. There’s the World Network of Users and Survivors of Psychiatry, a more institutional reform group with similar goals. There’s also the National Empowerment Center, cofounded by Chamberlin, with its emphasis on the recovery and peer-support model. Some of those in this movement call for more attention to trauma-centered care; some desire the abolition of certain psychiatric labels (like the “Campaign for the Abolition of Schizophrenia Label”); some call for a model of care not reliant on the DSM or medical professionals at all; some offer alternatives outside of psychiatric institutions (like crisis houses, or peer respite); while others propose to include newer diagnoses formed in collaboration with those with lived experience as a kind of harm-reduction. All are united, despite some major differences, under the same banner as the disability movement with which the mad movement shares so much: “nothing about us without us.” Listening to mad survivors of psychiatry or trauma teaches us to always be alert to the intricate maneuvers of power in our language and behavior. When the mad say “respect us”, what do you hear? A howl from deep within a noxious imbalance of chemicals being badly managed, or the cry from a potential friend who has suffered greatly to be treated with dignity and grace?
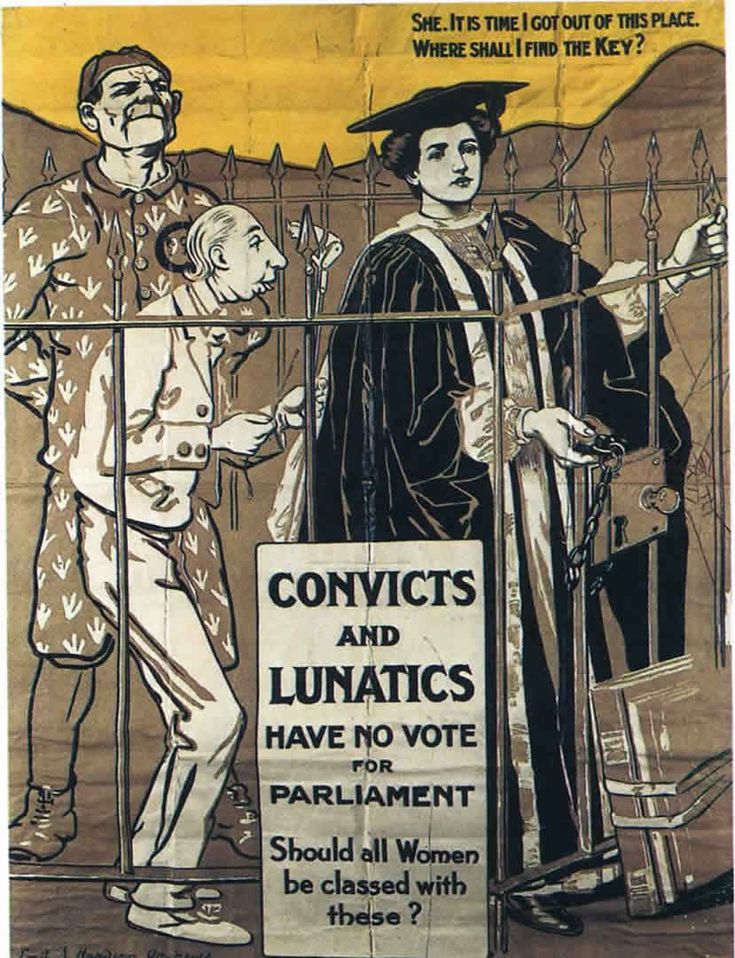
The mad share a natural solidarity with all those who have at one time or another been excluded from the process of civilization, rendered speechless and placed into the position of an animal. We can be more emphatic here: a disproportionate amount of those called and labeled mad have been black, indigenous, women, queer, or Othered in some manner. The mad at times have served as a convenient scapegoat for those desiring more political representation, a way to say “we are reasonable, we are not like those mad savages” as in a 19th century British propaganda poster for the suffragettes which shows a prisoner and a “defective” in a cage with a woman with the text “Convicts and lunatics have no vote for parliament, should women be classed with these?” When we respect madness and refuse to minimize or exclude it out of fear, we can better see how these exclusions support and necessitate one another. We can learn how the games of power compel us to destroy one another.
Our questioning of psychiatry should not lead anyone to believe that we intend to efface the experiences of extreme suffering sometimes called “madness”, or deny these possibilities to anyone. To the contrary, only by truly listening to the stories of the mad can we become more sensitive to such sufferings, experts of suffering, psychonauts more capable of sailing into the darkest corners of the human experience and come back stronger for it. For me, pushing back against psychiatry gives us more space to be sensitive to eccentricity of expression and a wider variety of emotional or mental reactions to life’s difficulties. Anyone could learn from the coping strategies of the mad. We are experts of the extreme.
Psychiatric discourse is full of convenient circles: because you are suicidal, you are mentally ill; because you are mentally ill, you are suicidal. Or: because you are psychotic, you are unintelligible; you are unintelligible because you are psychotic. Within the circle, there is no possibility of escape for those caught within, and no possibility of nuanced understanding, or careful practice for those lucky enough to evade its ever-growing span. The mad, and I speak with them, need to be able to speak about the voices we hear and the visions we see that others don’t without them reacting with fear and repulsion, without the banal refrain “have you seen a doctor about this?” being the only possible response, which is both an act of erasure and a threat (“if you don’t contact a doctor perhaps I will, or the cops”, etc). Listening to the mad means practicing a new radical form of listening: one in which we must come with curiosity and patience to the other, despite how far away they may seem, rather than dragging them to us in their moment of crisis. This may take hours, days, or months. We need patience because many of us are reacting to past violence, abuse, and trauma in our lives. These scars can be deeply buried, and confusedly expressed in moments of difficulty, sometimes woven into intricate and detailed symbolic systems opaque to the uninitiated. Self-care strategies that emphasize returning to a balanced homeostasis miss the fact that sometimes we need space to be mad, we need to go through crises or ecstatic reveries in a safe environment to process trauma or to reach a different stage of our development. We need elastic patterns of response to replace the rigid ones now in place. Psychiatric and trauma survivors say, as Jacqui Dillon does, that the question is not “what’s wrong with you?” as the doctors ask, but “what has happened to you?”

The jacket of Agnes Richter, a German psychiatric patient
Not everyone who has been labelled “mad” (or who sees themselves as such) has or wants a relationship, positive or negative, to a medical model at all, but see madness as a spiritual process, a muse, the call of the ancestor, see themselves as host to nerve fibers or waves of radiation or perhaps even the mysticism of cats to which no one else is sensitive. What could madness mean distinct from psychiatry? How do we mad people find each other outside of its networks? What do we share in common besides shared trauma or suffering? What do we have to offer each other beyond mutual support? One approach has been to take something which is thought of as a “symptom” and make it into the grounds for social and political organization.
The International Hearing Voices Network is one such group. The network began in the 1980s when, in the Netherlands, Patsy Hage, a distressed voice hearer, began to talk more and more about her suicidal thoughts with her psychiatrist Marrius Romme. She wanted to talk about the voices and what they were saying, but Romme had been taught that their words are meaningless. She noticed a cross on the wall. “Why shouldn’t you believe in the voices I really hear” she asked Romme, when “you believe in a God we never see or hear?”
Calling oneself a “voice hearer” has a very different ring than “schizophrenic” or “bipolar with psychotic episodes”, and is productive of an entirely different conception of the self and that selfs place in history. Shamans, religious or spiritual mystics and prophets including the Jewish mystic Isaac Luria, the Christian mystics William Blake, Joan of Arc, and Margery Kempe, the slave who fomented an insurrection Nat Turner, and the prophet Mohammad all reported hearing voices and seeing visions, as did writers Virginia Woolf, Bessie Head, Charles Dickens, Philip K. Dick; so too do many children report hearing the voices of imaginary friends; and adults the voice of a recently deceased loved one. Talking about “voice hearers” creates a broad continuum of experience rather than a category of pathological individuals. Mad Pride groups and The Icarus Project also take the time to explore creative ways to think about experiences typically seen as symptoms of madness, but with different emphases.
There are in-between spaces and groups with practical aspirations like the crisis houses and peer respite centers of the past and present like Kingsley Hall in England, Afiya in Massachusetts, and the Run Away House in Germany where patients make the important decisions, and live without fear of punishment or diagnostic stigma. Would thousands of people still be funneled in and out of hospitals during crises in the Twin Cities if we had more such spaces where former patients, mad people, and their friends were free to pass through their extreme distress or creative reveries in a supportive environment? What sort of space facilitates learning and growth through crisis rather than feelings of desperation and illness? Let us create spaces from which we will emerge from our crises and say the words Gerard de Nerval, the famous lobster-walking mad man of Paris, did following his crisis
The way I had been cared for brought me back to the affections of family and friends and I was able to judge with greater sanity the world of illusion I had lived in for a while. All the same, I feel happy over those convictions I have acquired and I compare this series of trials I went through to that ordeal which, for the ancients, represented the idea of a descent into hell.
We must listen to the voices of the mad for, while there may be some usefulness in looking at statistics, we often place too much emphasis on their importance. While it’s true that statistics may tell us of the effectiveness of a certain treatment, or of negative side-effects of a drug over time, they cannot tell us what these interventions mean to a person with a past, a present, and a future, friends, family, loves, fears, hopes, desires; they cannot tell us anything about what madness means to those experiencing it; they cannot tell us why people believe they have the experiences that they have. Listening to people tell their own stories in their own ways gives us access to information that can never be obtained within the limits set by scientific research. Even if the research were all correct and supported by evidence, understanding the science behind madness does not mean that you understand madness, just as understanding how the brain processes and synthesizes the scenes of a film does not grant one access into the meaning of that film.
The radical diversity of madness narratives speaks to the need for the fostering of what Martin Luther King Jr. called spaces for “creative maladjustment”. The experiences of those called mad and their explanations for it do not form a cohesive system. To approach this, we need elastic, adaptable frameworks. The mad already have these, by and large, because we have to bend and twist our speech and thinking so far to make the public comfortable, to not show our scars, our grand ambitions, our connections to things unseen, lest we be locked up in hospital again. The problem with both the psychiatric model and the individual self-help model is that they tend to impose a set of universal beliefs on the one in need of help. If I were to say “I hear voices, sometimes wonderful, other times horrific, because I have a connection with spirits of the past”, this imposes nothing on the other, but yet is still something sharable. I can share their words, their wisdom, their pain. Setting aside whether it is true or false, to tell me in this case “this is the effect of a failure of your dopamine inhibitors” is to collapse all meaning and reduce it to the interplay between some chemicals in a body. It implies all those who adopt different frameworks for themselves are essentially deluded. Despite good intentions, this explanation is imperial, and, when expressed, excludes all other possibilities under the warlike banner of “chemical imbalance”.
The problem is not that some people find meaning in a diagnostic label, but that such self-identification is presented as the only possibility for those among us who regularly undergo crises or unusual experiences. Ask yourself: what means do we have today or what means do I myself offer my friends for legitimating suffering, extreme states, ecstasy or voice hearing without passing through a medical model, without saying “his art is beautiful, it’s amazing what bipolar people can do” or “She’s such a great person, it’s so sad what people with schizophrenia have to suffer through.” How many people choose to identify as “depressives” or “schizophrenics” not because it is the best possible option for them, but because it is the only one they are aware of, and the only one which anyone else will take seriously? How can we say “I believe you” without also implying “I also believe you are ill”? Listening to the mad and respecting the frameworks in which the mad think does not entail a rejection of responsibility and closure away from others into the world of fantasy, but the opposite. Nothing for me is more closed-off to sharing than the abstractions of brain chemistry, no choice or responsibility is granted me when my choices are merely effects of my brain malfunctioning.
To finish, I’d like to read a poem by Emily Dickinson:
Much Madness is divinest Sense-
To a discerning Eye-
Much Sense-the starkest Madness-
‘Tis the Majority
In this, as All, prevail-
Assent- and you are sane-
Demur- you’re straightway dangerous-
And handled with a Chain-
Much Madness is divinest Sense-
To a discerning Eye-
Much Sense-the starkest Madness-
‘Tis the Majority
In this, as All, prevail-
Assent- and you are sane-
Demur- you’re straightway dangerous-
And handled with a Chain-
Revelation, beauty, suffering, energy, silence, violence, abuse, politics, fear: such is the company the mad find themselves with when they board the ship of fools we call madness. When you spot it coming on the horizon, full of dancing, drinking, screaming, tattered and broken souls, will you let it dock, and rest, perhaps even board it for a while as we travel down the river, or will you hide beneath the covers, turn off the lights and hope we don’t notice you as we pass?
CLOSING
Sasha again. I want to take just a second to tell you about a bibliography and study guide I put together around the materials introduced in this talk. It’s separated into 10 units on mental health, madness, and psychiatry, and designed for you, the reader, to add, subtract, mix and match, take or leave anything included. There’s readings, podcast episodes, artworks, movies, websites, and resources listed, along with summaries of each text, and questions for you or a reading group to consider. Every unit includes at least one text written by someone who has been identified as or personally identifies as “mad”. The study guide is free, as are all the texts included. Find it on the front page of our website belliresearchinstitute.com
S o n g s u s e d:
Fizz “Submarine Intro”;
King of Hearts Sountrack “La Valse Tordue”;
2 tracks produced and mixed by Sasha Durakov;
Bud Powell “Polka Dots and Moonbeams”;
Annie Ross “Twisted”;
Luboš Fišer “Valerie a týden divů”
* Header image is The Maze by William Kurelek
Comments
Post a Comment